MRSA guideline – HIS and IPS guideline
Universal or targeted screening
- Targeted or universal screening, linked to specific action – isolation and/or decolonisation.
- If targeted screening is undertaken, define the risk factors for MRSA.
Rescreening
- Routine rescreening is not recommended.
- Do not perform rescreening for those who are positive on admission unless decolonisation therapy is used.
- If decolonisation was undertaken, retest 2-3 days after completion of decolonisation.
- Rescreen a previously negative patient if there is significant MRSA exposure or locally assessed risk of late acquisition.
Test
- Swabs should be taken at least from two different sites depending on presentation (nose, perineum, device entry sites, wounds, urine, and sputum).
- Use either PCR or traditional culture methods for MRSA screening as you consider appropriate, depending on the local laboratory facilities.
- If using PCR methods, maintain access to culture methodology for specific circumstances such as outbreak investigation or sensitivity testing and support molecular technologies.
Staff screening
- Do not routinely screen staff.
- Screen staff if there is an epidemiological reason for suspecting a staff member as a source of MRSA (if transmission continues on a unit despite active control measures, if epidemiological aspects of an outbreak are unusual, or if they suggest persistent MRSA carriage by staff).
- If possible, involve the Occupational Health Team in the process of staff screening and management.
- Screen staff at the beginning of their shift to avoid mistaking transient carriage for persistent carriage.
- Screen anterior nares and any areas of abnormal or broken skin.
- For staff who test positive, consider additionally screening the throat, hairline, and groin/perineum.
- Staff with nasal carriage only offer decolonisation; exclusion is not necessary.
- Staff with infected lesions/ skin rash, offer decolonisation, redeploy in a low-risk area/consider excluded from work.
- Staff with persistent carriage -consider excluding staff from work, reduce patient interaction, offer decolonisation, consider risk factors for colonisation, and investigate persistent carriage in a multidisciplinary team to determine any associated factor.
- Develop local policies to guide the decision of when staff should be excluded from work and when they should return, taking into consideration the individual’s risk of transmission to patients (e.g. a staff member colonised with MRSA who is working in an ICU or neonatal unit represents a greater potential risk to patients than a staff member with MRSA working in an outpatients’ department).
Decolonisation
- Use mupirocin for nasal decolonisation, either selectively (i.e., for those who are colonised) or universally (i.e., for all high-risk patients).
- Use chlorhexidine, either selectively or universally, for body decolonisation to reduce MRSA carriage.
- Consider alternatives (e.g. octenidine) where mupirocin and chlorhexidine are not feasible.
- Monitor the emergence of resistance, especially to mupirocin and chlorhexidine, if used extensively.
- Follow manufacturers’ guidance when using decolonisation products.
- For skin decolonisation, if 4% chlorhexidine wash is used, moisten the skin, apply the wash, and leave for 1–3min before rinsing off; if 2% chlorhexidine wipes are used, do not rinse off.
- For skin decolonisation, pay special attention to known carriage sites such as the axilla, groin, and perineal area.
- After each bath and wash, provide clean clothing, bedding, and towels.
In patients with eczema, dermatitis, or skin conditions – an attempt should be made to treat underlying skin conditions. A dermatology consultant could be consulted. Alternatives are – Oilatum bath additive or Oilatum plus (with added benzalkonium chloride 6% and triclosan 2%).
Mupirocin prolonged or repeated use may lead to resistance. It should not be used for two courses for 5 days.
Standard/contact precaution, isolation
- Use standard infection prevention and control precautions.
- Contact precautions for direct contact with the patient or their immediate environment.
- Gloves and aprons must be changed between care procedures and hand hygiene must be performed after glove removal.
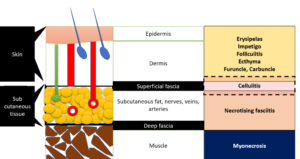
- Consider placing colonised/infected patient in a single room, based on risk assessment – consider the risk of transmission associated with the patient’s condition and the extent of colonisation or infection (e.g. sputum, exfoliating skin condition, large open wounds) and the risk of transmission to other patients in the specific care setting, e.g. in burns units.
- If other demands on single-room use take priority, alternative strategies such as nurse cohorting may be appropriate. Use decolonisation therapy to temporarily suppress MRSA and prevent transmission to other patients.
- Prioritise room cleaning and disinfection for MRSA patients placed in isolation or on contact precautions.
- Be consistent in the use of protective equipment to ensure that patients have confidence in the decision to place them in isolation.
Transfer:
- Do not transfer patients between wards, units, hospitals, or other clinical settings unless clinically necessary.
- Inform the receiving ward/unit/care home and the ambulance/transport service that the patient is colonised/infected with MRSA.
- MRSA colonisation is not a barrier to discharging patients to another health care setting, their home or residential care.
Share equipment
- Clean and disinfect shared pieces of equipment used in the delivery of patient care after each use, utilising products as specified in a local protocol.
- Every healthcare worker should know the importance and their specific responsibilities for cleaning and decontaminating the clinical environment and the equipment used in patient care.
- Introduce policies for staff, patients, and visitors to clean their hands before and after they use the shared equipment.
Surveillance
- Undertake surveillance as per local infection prevention and national policy.
- Consider using local surveillance of MRSA acquisition (colonisation and infection) as a component of local strategies to prevent and control MRSA and to drive improvement where needed.
Children
- Consider using chlorhexidine in neonates only if there is no alternative and there is no broken skin present.
Environmental sampling
- Routine sampling is not recommended.
- Screening/sampling can be done as part of a targeted investigation of an outbreak.
- Continue using currently utilised products approved for use in healthcare.
- Consider hydrogen peroxide vapour (HPV) or ultraviolet (UV-C, PX-UV) devices as an adjunct to terminal cleaning as a part of a wider IPC strategy.
Information
- Make patients aware of the reasons for MRSA screening and decolonisation.
- Inform patients of their screening result as soon as it is available.
- Provide information in a format and language that the patient and their family can understand.
- For patients who are identified as MRSA-positive, provide consistent and appropriate information about:
> The difference between colonisation and infection
> The microorganism
> How MRSA is acquired and transmitted
> How MRSA is treated
> The reasons for contact precautions or isolation. - Provide clear information to patients about the need for the use of protective equipment to reduce feelings of stigma.
- Advise visitors about the need and available facilities for hand hygiene.
- Where applicable, advise visitors about the use of gloves and aprons.
- On discharge, provide consistent and appropriate information about the following:
> The risks to household members, friends, and family.
> The implications for future health and health care.
> Persons who need to be notified about their MRSA colonisation status.
> If applicable, instructions on the decolonisation regimen with the information that the results may not be permanent. - Make healthcare workers and patients aware that decolonisation therapy does not necessarily result in complete eradication but that achieving temporary suppression is sufficient in many circumstances.
- Inform patients about the possibility of re-colonisation and the importance of changing linen, towels, and clothes daily.
Deceased
- Follow national guidance for managing infection risks when handling the deceased.